Lymphedema is a common condition that develops after breast cancer treatment. Unfortunately, there is no cure, but there are many products and practices that can help patients manage their lymphedema.
Key Takeaways
- Lymphedema is swelling caused by fluid buildup in lymph vessels.
- Breast cancer surgery or radiation therapy can damage the lymph system and cause lymphedema.
- Massage and compression therapy are two effective ways to manage lymphedema.
Table of Contents
What is lymphedema?
What is the likelihood of developing lymphedema after cancer?
What are the symptoms of lymphedema?
What is the difference between post-operative swelling and lymphedema?
What factors increase the risk of lymphedema?
Ways to Reduce the Risk of Lymphedema
Lymphedema Management
Top Products in This Article
What is lymphedema?
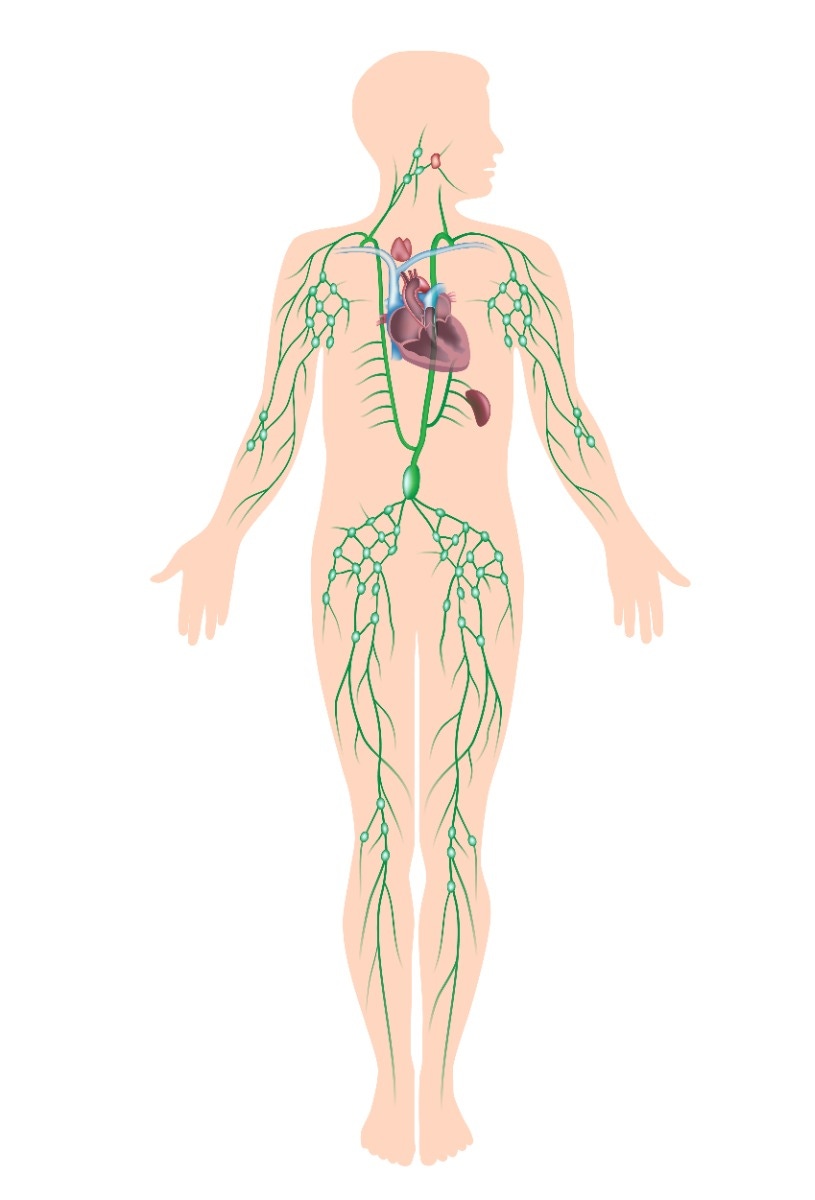
Lymph vessels run throughout the body, much like blood vessels. They absorb lymph fluid from the tissue and move it to the lymph nodes to be filtered. During breast cancer surgery, some lymph nodes may be removed to check for cancer cells. Radiation therapy can also damage the lymph system and lead to blockages.
Both procedures can cause fluid to build up and cause swelling (edema). The swelling can be large and uncomfortable. This secondary lymphedema often occurs in the chest area or the arm, due to the location of the lymph nodes that are damaged.
What is the likelihood of developing lymphedema after cancer?
The statistics vary based on different research and studies. One study that followed 631 breast cancer patients over 5 years found that 42% developed lymphedema (23% mild, 12% moderate/severe, 2% chronically moderate or severe)5.
Another study looked at rates depending on dissection. The sentinel lymph node biopsy (SLNB) – which removes fewer nodes – is employed whenever possible and is associated with lower lymphedema risk (3%)3. In some circumstances, however, a greater number of lymph nodes must be removed through axillary lymph node dissection (ALND) and the lymphedema risk is higher (19%)3.
What are the symptoms of lymphedema?
- Swelling in the arm, chest, armpit, or hand
- Jewelry, clothing, or bras may feel tighter than usual
- Feelings of tightness or heaviness in the upper limb
- Thickening or firmness of the skin on the affected area
- Decreased flexibility in the shoulder, elbow, wrist, or fingers
- Weakness or fatigue in the arm
What is the difference between post-operative swelling and lymphedema?
Some swelling, also known as post-operative edema, can occur after surgery or during and following radiation therapy. This should decrease in the weeks immediately after treatment.
It’s important to obtain baseline measurements from your patients – either before surgery or immediately after – to help you learn how to identify early signs of lymphedema (chronic swelling). Encouraging patients to be active after surgery can help in their recovery process.
What factors increase the risk of lymphedema?
- Removal of a large number of axillary lymph nodes
- Radiation therapy to the axillary lymph nodes
- Cancer cells many axillary lymph nodes
- Infection in the area after surgery
- Obesity
- A severe injury, like a serious burn or wound, to the affected arm
- Genetic predisposition
- Recurrent tumor
Factors that Don’t Appear to Increase the Risk of Lymphedema
The type of surgery (lumpectomy vs. mastectomy) doesn’t seem to impact the development of lymphedema. Whether or not a woman has reconstructive surgery after a mastectomy and the type of breast reconstruction chosen also doesn’t affect the risk of developing lymphedema6.
Ways to Reduce the Risk of Getting Lymphedema
Avoiding injury after surgery is essential. Infections, burns, or injuries cause the body to respond by sending extra white blood cells in fluid to the area. Missing or damaged lymph nodes can have a hard time moving this extra fluid, which can trigger or worsen lymphedema. Since injury can’t always be avoided, here are some guidelines.
These tips can help reduce your risk:
- Blood draws, shots, and IVs should be done in the unaffected arm (when possible)
- Blood pressure should be taken on the unaffected arm, if possible
- Encourage regular, low-impact exercise
Skin care tips:
- Keep the area clean and use a moisturizing lotion regularly
- Clean and protect any open areas (cuts, hangnails, scratches, etc.)
- Wear sunscreen with at least 30 SPF daily
- Avoid cutting cuticles, push them back with a cuticle stick instead
- Wear gloves when gardening, doing yard work, working with harsh chemicals, or using steel wool
- Use insect repellent to avoid bug bites
- Be careful when shaving the underarm, consider using an electric razor
- Wear a thimble if sewing to avoid needle pricks
- Keep pets’ nails short to avoid scratches
Avoid extreme temperatures:
- Avoid high heat areas, like hot tubs and saunas
- Patients should test water with their unaffected arm before bathing – the affected arm might be less sensitive to temperature than it used to be
- Avoid tight or heavy jewelry or clothing with constricting elastic
- Avoid using shoulder straps on the at-risk side when carrying briefcases or purses
- Recommend wearing a compression sleeve during air travel
Lymphedema Management
Lymphedema management is an important step for a patient’s well-being and quality of life. Diuretics (water pills) won’t relieve the swelling because it’s lymph fluid, not water. However, swelling can be reduced through a treatment regimen called complex decongestive therapy (CDT).
Massage
Massage is the first step to reduce swelling. The specific massage manipulation used for lymphedema is called manual lymphatic drainage (MLD). MLD stretches the tissue to increase the flow of lymph fluid through your patient’s system and reduce swelling. The strokes should be gentle and slow during decongestion. A flexible measuring tape can help you track reductions and fluctuations in swelling.
Share this example of a MLD self-massage with your patients!
Compression
Compression can also help you maintain the reductions in swelling. Lymphedema from breast cancer treatment commonly occurs in the arm, but it can also affect the chest. Compression can be used on both of these areas. Multi-layer bandaging is often used first, while a garment might be used after the lymphedema is better controlled.
Multi-Layer Compression Bandaging
The multi-layer compression bandaging process uses a variety of bandages to provide even compression, which reduces the amount of fluid that can accumulate. Begin wrapping distally (near the fingers) and continue proximally (toward the heart) with even tension. The size of the bandages is specific to create a variable pressure and move fluid out of the limb.

Layer 1: Skin Protection
- tg tubular stockinette
- Stockinettes provide skin protection and absorb perspiration.
Layer 2: Fingers/Toes
- Mollelast
- Individually wrap the fingers and toes to help prevent the swelling from spreading.
Layer 3: Padding
- Cellona Synthetic Padding
- Padding cushions the arm and ensures the pressure is distributed evenly.
Layer 4: Focal Compression
- Komprex Foam Rubber
- Closed cell foam focuses pressure on tough fibrotic tissue or problem areas. Grey (open cell) foam is used for cushioning the entire limb or adding mild pressure.
- Swell Spots
- Soft, washable Swell Spots are another option for compression. Many of them can also be used in a compression bra. They help reduce swelling, scarring, and fibrotic tissue.
Layer 5: Short Stretch Bandages
- Rosidal K
- Short stretch bandages give high working pressure and low resting pressure. These provide the compression needed in multi-step bandaging. Highly elastic bandages like ACE bandages should not be used, since their high resting pressure makes them hard to tolerate and allows fluid to enter.
Layer 6: Tape
- Silkafix Tape
- Tape secures the bandaging in place. Avoid using clips because they could puncture the skin and lead to infection.
Consider buying a bandaging kit so you have everything you need for bandaging. Each kit comes with two sets, so patients can wash one and wear the other.
Compression Garments
Garments are often worn when your lymphedema is better controlled. They still provide compression but are easier to don than bandaging. ReadyWrap Arm and ReadyWrap Gauntlet are simple ways to get the compression patients need during the day.
Check out this video to see how easy ReadyWrap garments are to put on!
Try the Caresia MCPs to Axilla Garment for full coverage for compression at night. Wearing compression garments while resting or sleeping helps prevent fluid buildup so patients can easily don their day garments when they wake up.
Or use a foam elevator to support and elevate the limb while resting (no need to elevate if the limb is compressed).
Exercise
Research has shown that exercise does not increase your patients’ risk of lymphedema4. In fact, moderate exercise might offer protection for real-life situations like carrying groceries or lifting a child. However, obesity increases the risk of lymphedema, so exercise and healthy eating are important to help avoid lymphedema.

“Inactivity puts patients at a greater risk than over-exertion.” - Sarah Stolker, MSPT, CLT-LANA
If a patient has lymphedema, they should wear a compression sleeve during exercise. Start at a low intensity and slowly increase over time. Resistance bands are an easy way to work the upper extremities while controlling the resistance.
Recap
While lymphedema doesn’t have a definitive cure, there are plenty of ways to manage the swelling, including massage and compression therapy. Protecting the skin, avoiding extreme temperatures, and promoting circulation are all helpful ways of reducing a patient’s risk of lymphedema.
References
- American Cancer Society. (2016). For People at Risk of Lymphedema. https://bit.ly/2tuDXqG
- American Cancer Society. (2016). For People With Lymphedema. Retrieved from https://bit.ly/2tt8llx
- American College of Surgeons. (2013). Breast Cancer Patients’ Fear Exceeds Risk. Retrieved from https://bit.ly/2KnutY3
- National Cancer Institute. (2015). Lymphedema (PDQ®)–Health Professional Version. Retrieved from https://bit.ly/2KjbDOA
- Norman, S. A., Localio, A. R., Potashnik, S. L., Simoes Torpey, H. A., Kallan, M. J., Weber, A. L., … Solin, L. J. (2009). Lymphedema in Breast Cancer Survivors: Incidence, Degree, Time Course, Treatment, and Symptoms. Journal of Clinical Oncology, 27(3), 390–397. http://doi.org/10.1200/JCO.2008.17.9291
- Susan G. Komen. (2018). Lymphedema. Retrieved from http://sgk.mn/2rFdQPx
Medical Disclaimer: The information provided on this site, including text, graphics, images, and other material are for informational purposes only and are not intended to substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other healthcare professional with any questions or concerns you may have regarding your condition.







 US
US France
France Australia
Australia




